AI-Powered Healthcare: Enhancing Patient Care and Outcomes
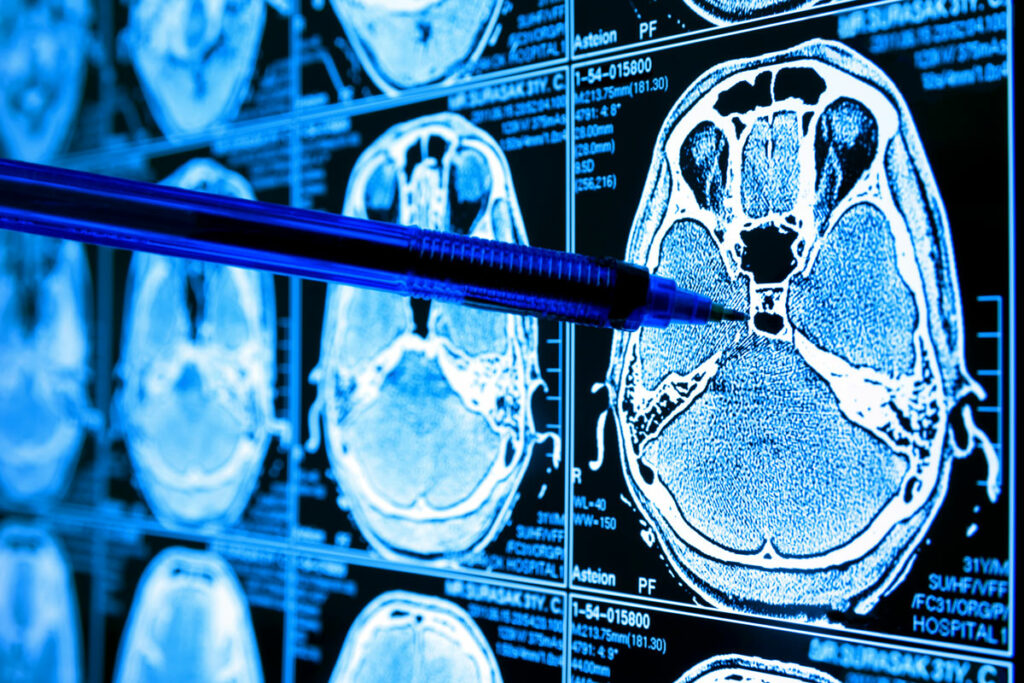

On any given day, a radiologist views hundreds of patient images — from X-rays to MRIs and everything in between.
While a highly skilled radiologist can see most issues quickly, some conditions are harder to diagnose. Tired eyes might even miss potential stroke warning signs — a condition often seen in MRI imaging.
Thanks to artificial intelligence (AI), that same radiologist can get a high-stroke-risk patient’s images pushed to the top of their viewing queue to get them the care they need faster.
That’s exactly one of the ways AI is being used at AdventHealth, says
Rob Purinton, AdventHealth’s vice president of analytics and performance improvement.
In 2020, AdventHealth rolled out formal AI in imaging departments to assist radiology departments in offering more efficient patient care.
“It really has helped us to identify things like stroke faster,” he says, noting that typically a radiology tech captures the images and then the doc sits and looks it over. “Time is brain matter in a stroke. We want to respond as quickly as possible.”
A recent New Economic Forum report shared that AI’s highest application potential in healthcare includes AI-driven diagnosis, infectious disease intelligence, and clinical trial optimization.

Likewise, other healthcare systems in Northwest Florida are adopting AI usage, too, for better patient outcomes.
Last year, Baptist Health announced its use of Hyro, which uses AI assistants to enhance the patient and team member experience. The hope is its use will minimize the time Baptist personnel need to tackle repetitive tasks such as password resets. Earlier this year, the University of Florida College of Medicine – Jacksonville shared its decision to use Paige’s full AI portfolio across prostate and breast cancer cases for diagnostic efficiency and accuracy.
While AI tools are helpful and exciting to embrace, Purinton and his team are cautious about which ones make it into the healthcare setting. It’s essential that patient security and privacy are at the forefront of those decisions, he says.

“We’re not just throwing generative AI into healthcare,” says Purinton, who notes all AI vendors must pass rigorous exams. ”We rejected an AI tool this summer because the data was going overseas for storage. We had enough concerns about the security of data, so we passed on that one. We have to look under the hood and see where data is going and how it’s being used and stored.”
Given how many patients most doctors have, that’s a lot of data that AI can easily sift through to make a physician’s job much easier.
Dr. James Grimes, in Saint Johns, enjoys using AI for the efficiency of patient care that integrates their past medical history into their current health situation. His practice uses robotics, computer navigation, radiologic modalities and AI throughout any given day.
“AI allows for the ability to coordinate care across different fields such as orthopedics, cardiology and medicine — this provides for a more streamlined and efficient outcome for each patient,” he says.
With all of the efficiencies AI brings to healthcare, does this mean the replacement of well-trained doctors and nurses? Dr. Grimes doesn’t think so.
“I do not believe any physician feels that AI will completely replace us in terms of medicine because well-trained and experienced physicians have a “sense” of things that we do not believe will be able to be transported to AI,” he explains. “We certainly do welcome AI in practices and enjoy its benefits in terms of improved patient care at a more efficient level, which allows for improved health care with less cost to the system or patient.”